Climate change is the largest public health emergency of the 21st century, threatening humanity's access to food supplies, safe drinking water, clean air and shelter (World Health Organization (WHO), 2023). Since the 1800s, the main driver for climate change has been greenhouse gas emissions (GHGE) produced by human activity (UN, 2023). These emissions blanket the earth, trapping the sun's heat, which results in global warming. It is not too late to alter these effects and governments around the world are tasked with the challenge of reducing emissions to reverse the devastating effect our lifestyles are having on our health and our planet.
In the UK, the government aims to achieve net zero GHGEs by 2050 (Department for Business Energy and Industrial Strategy, 2019). The NHS produces 23 megatons of carbon dioxide equivalent (CO2e) per year, which makes it the largest emitter of all the UK public sectors; and 3.5% of this is produced by pressurized metereddose inhalers (pMDIs) (Janson et al, 2020). This type of inhaler uses hydrofluorocarbon (HFA) propellant to deliver a measured amount of medication to the lungs in a short sharp burst. While this is an effective delivery method of inhaled medication, HFA propellants omit high levels of CO2e. To put this into perspective, using one inhaler has the same global warming effect as driving a car for 170 miles (National Institute for Health and Care Excellence (NICE, 2019).
In broad terms, there are two main types of inhalers: pMDI and dry powder inhalers (DPI). DPI devices contain no propellant so their global warming potential (GWP) is significantly lower (MacKenna, 2019). However, 70% of the 3.9 million people in the UK with a diagnosis of asthma are managed with pMDIs, which is higher than any other country. Switching just 10% of pMDI to DPI has the potential to save around 68.8 kilotonnes of CO2e each year, making this a prudent area for change (Wilkinson et al, 2019).
Various guidelines have been published by government and respiratory societies in recent years encouraging inhaler changes (NHS Sustainable Development Unit, 2016; British Thoracic Society (BTS), 2017; Environmental Audit Committee, 2018; NHS England, 2019). However, despite these recommendations, attempts to promote and achieve targets at a local level have been slow. As a result, integrated care boards (ICBs, formerly clinical commissioning groups) have applied a Prescribing Incentive Scheme to encourage the change from pMDI to DPI in primary care.
The scheme offers general practices financial reward when using medicines optimisation, cost-effective and high-quality prescribing (NHS Bedfordshire, Luton and Milton Keynes Clinical Commissioning Group, 2021). However, there is now pressure in many local areas to achieve this via unconsented blanket inhaler changes. While this may produce fast results in the short term, the approach is not patient-centred and has been linked to several negative outcomes in clinical, economic and environmental scenarios (Chakma and Usmani, 2022).
Aims and objectives
The primary aim of this review was to establish how to implement sustainable inhaler changes without compromising patient care and disease control in the primary care setting. This includes a review of how to switch pMDI to DPI effectively, as well as exploring other areas for change, including recycling and altered prescribing habits.
Literature search
The search was conducted in January 2023 using Discover and PubMed search engines. Search terms were ‘environmental impact’ OR ‘sustainability’ OR ‘carbon footprint’ AND ‘inhaler’. This offered a total of 437 results initially: 375 on Discover and 62 on PubMed. On Discover, it was possible to reduce the total number of articles down to 44 by narrowing down the date search to the last 5 years (2018–2023), only including peer-reviewed and academic journal types, only those written in English and by adding the search filter ‘Subject: inhaler’. A filter of the title was then completed by reading them and removing those that were not relevant.
On PubMed, it was possible to reduce the total number of articles down to 30 by narrowing the date search to the last 5 years again (2018–2023) and by filtering through the remaining titles by reading them and removing those that were not relevant to the research question.
This left a total of 74 reports. Once these had been filtered through and articles removed that were duplicates, not all available or were not primary research or high-quality systematic review, the final number of papers to be included in the literature review was 10.
Quality assessment and data extraction
Articles were assessed for quality using the Critical Appraisal Skill Programme (CASP) checklist system, which included randomised controlled trials, systematic reviews, qualitative studies, economic evaluation and clinical prediction rule checklists. The patient, intervention, comparison, outcome (PICO) framework was also used to help provide clarity when performing the literature search and to assist in achieving comprehensive and non-bias results.
A spreadsheet was created using Google sheets for the purposes of data extraction. Information was categorised under seven different headings: author and year; study design; population or target group; aims and objectives; outcome; significant results/conclusions; and study quality. By using this system it was possible to break information down into structured, manageable sections and highlight the types of paper that were being analysed, the relevance to the research question, a summary of the main results and key messages as well as identify the limitations of each paper.
» Sustainable inhaler changes offer a balance between disease control, patient health and environmental effects, and general practice offers the ideal platform to promote and apply these changes «
Results
The results are categorised under four main headings: comparative GHGEs of inhalers; recycling; inhaler selection; and disease control.
Comparative GHGEs of inhalers
There are three propellants available for use in pMDI devices:
Another propellant is in production that will have a very low GWP, possibly even lower than that of DPI devices (Wilkinson et al, 2019; Pernigotti et al, 2021). Due for release in 2025, it is estimated to produce just 0.7% of total GHGEs when compared with HFA-134a (Jeswani and Azapagic, 2019). Table 1 offers a visual summary of the varying levels of CO2e produced by commonly used inhalers, as identified from the literature search.
| Product name | Propellant used | Device type | Actuations per inhaler | CO2e kg per inhaler |
|---|---|---|---|---|
| Ventolin (SABA) | HFA-227ea | pMDI | 200 | 25.260* |
| Salamol (SABA) | HFA-134a diluted | pMDI | 200 | 9.870* |
| Salbutamol (SABA) | – | DPI | 60 | 0.600^ |
| Clenil Modulite (ICS) | HFA-134a | pMDI | 200 | 20.350 |
| Easyhaler Beclometasone (ICS) | – | DPI | 200 | 0.580# |
| Fostair (ICS/LABA) | HFA-134a | pMDI | 120 | 19.650 |
| Fostair NEXThaler (ICS/LABA) | – | DPI | 120 | 0.915> |
| Flutiform (ICS/LABA) | HFA-227ea | pMDI | 120 | 36.500 |
*Wilkinson et al, 2019; ^Janson et al, 2020; #Panigone et al, 2020; >Vinge et al, 2020
Inhaler selection
Inhaler changes must involve clinical assessment regarding need and appropriateness, followed by education and assessment of inhaler technique (Janson et al, 2020; Wilkinson et al, 2019; Woodcock et al, 2022). Change implemented without consent is associated with patient discontent, reduced disease control and reduced confidence in medication (Panigone et al, 2020; Pernigotti et al, 2021).
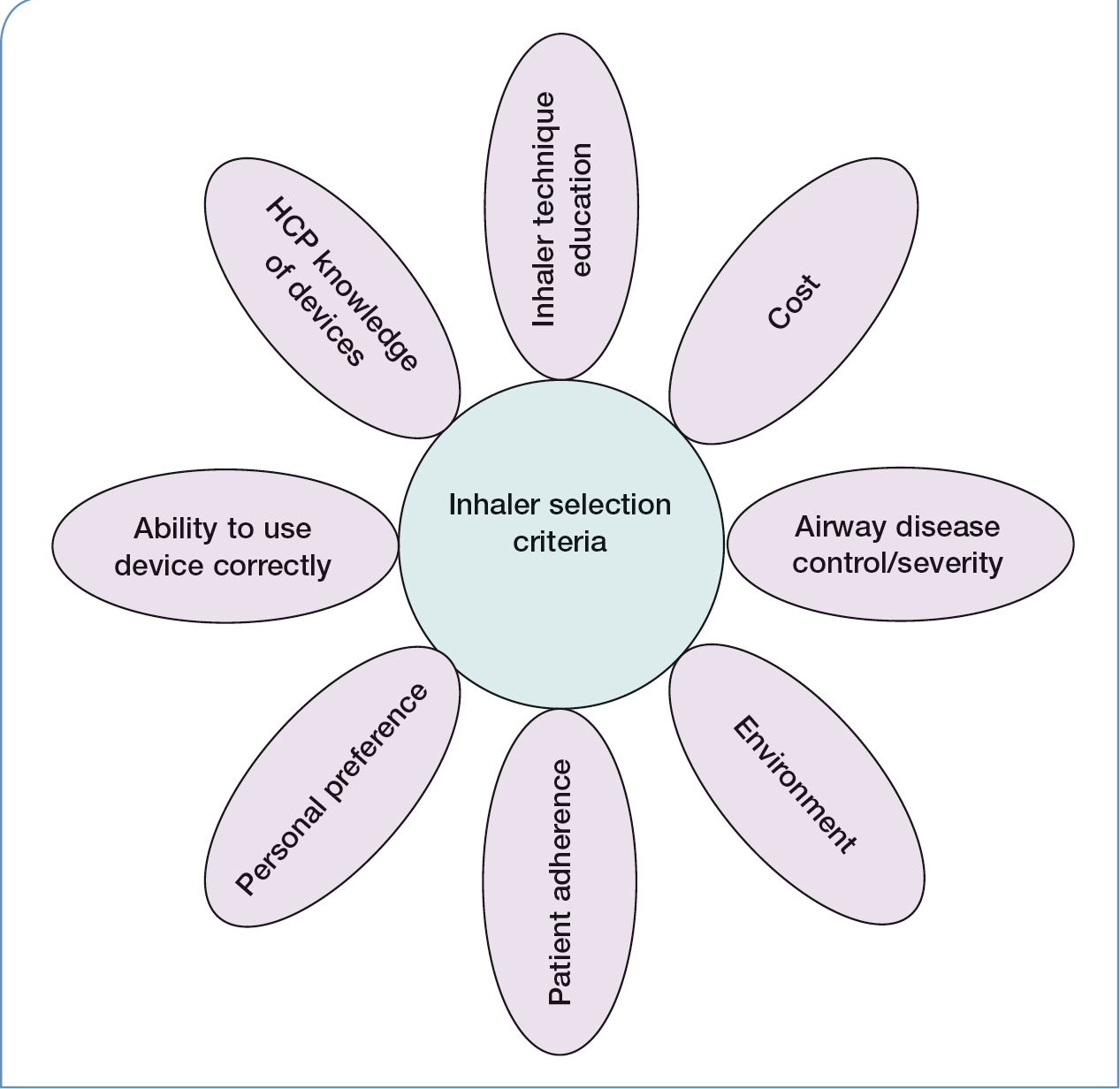
Forced inhaler changes offer the opportunity for more rapid results in the short term. However, the effect of these changes on lowering CO2e is ultimately lessened due to the associated poor control that links to an increased need for reliever medication and additional healthcare resources (Janson et al, 2020; Pernigotti et al, 2021). There were various key components to consider when selecting a new inhaler; Figure 1 offers a visual summary of these factors.
Altering the prescribed dosing of pMDI offers an opportunity to lower GHGEs. For example, by prescribing a higher strength of preventer pMDIs (i.e. switching from Clenil 100 to Clenil 200) and advising one puff twice daily instead of two puffs twice daily, it is possible to reduce carbon footprint potential (Twigg et al, 2019). In addition, there have been recommendations that ICBs remove Ventolin pMDI, Symbicort pMDI and Flutiform pMDI from their formularies, as these all use the most potent propellant HFA-227ea (Twigg et al, 2019; Wilkinson et al, 2019).
Poor inhaler technique is common and significantly reduces the effectiveness of inhalers. Real-life studies comparing pMDI and DPI techniques have found that DPIs have consistently been superior. This is due to ease of use, improved tolerance and fewer errors when compared with pMDI (Vinge et al, 2020; Woodcock et al, 2022).
Disease control
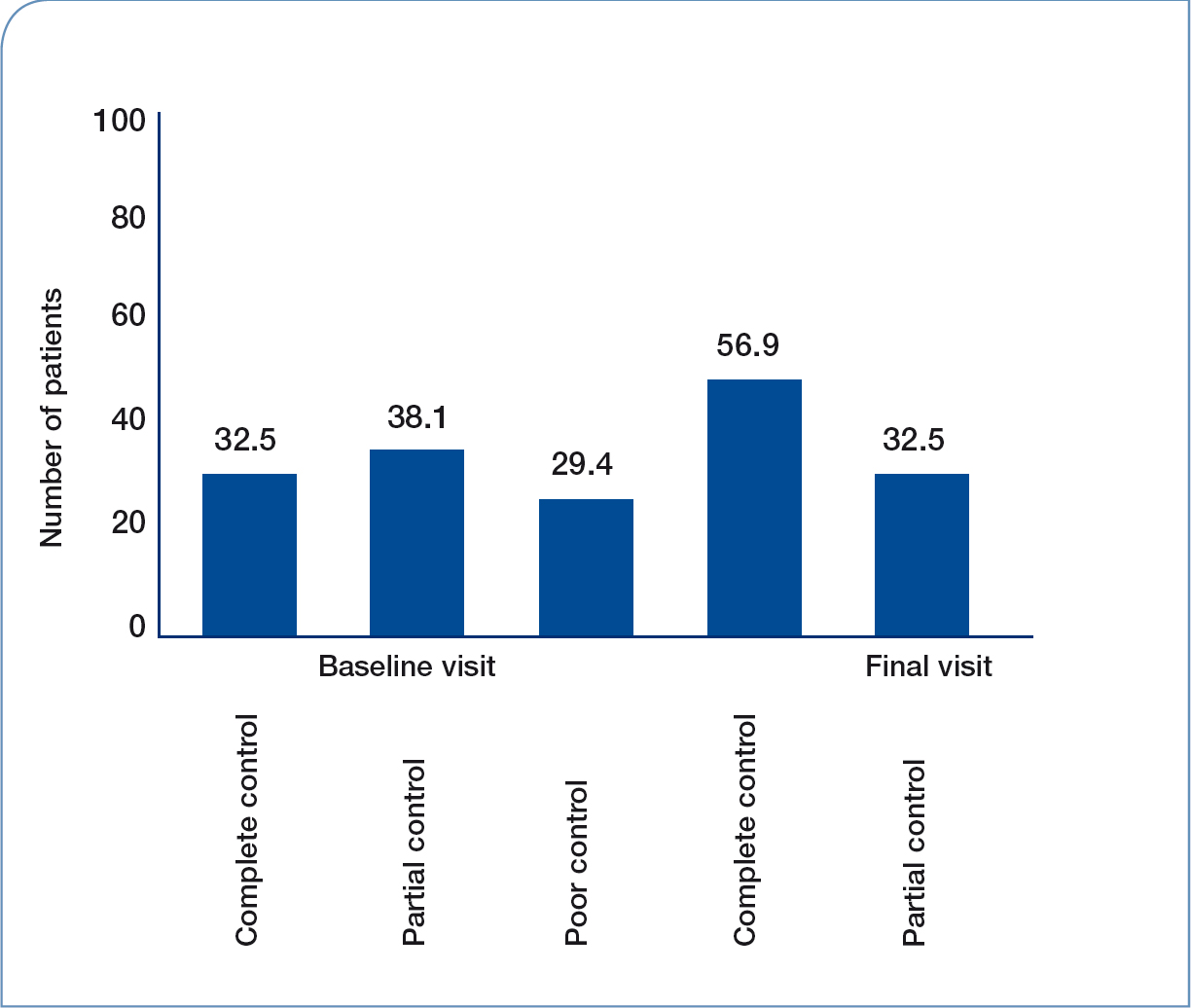
Improving asthma control leads to enhanced health outcomes, decreased need for extra health resources, reduced absence from work and reduced CO2e emissions (Wilkinson et al, 2019; Vinge et al, 2020; Kponee-Shovein et al, 2022). Studies showed that switching to DPI not only improved inhaler technique but also improved disease control (Wilkinson et al, 2019; Vinge et al, 2020). A post-hoc analysis of asthma outcomes from the Salford Lung Study in 2022 demonstrated a 50% reduction in CO2e emissions, and a reduction in prescriptions of salbutamol inhalers per year in those switched to DPI (Woodcock et al, 2022). In addition, Vinge et al (2020) conducted a 12-week non-interventional switch study using the Asthma Control Test (ACT) pre- and post-switch from their current inhaler to Easyhaler (DPI), which shows improved disease control (Figure 2).
Several different studies had also found Salbutamol DPI to be as effective in treating exacerbations as pMDI+spacer or nebulisers (Twigg et al, 2019; Kponee-Shovein et al, 2022). Exacerbation severity determines the amount of CO2e emissions, with levels increasing as severity increases (Pernigotti et al, 2021; Woodcock et al, 2022; Kponee-Shovein et al, 2022). Reducing the need for SABA inhalers through improved asthma control has the potential to reduce patients total annual CF by 17–48%.
Recycling
When the lifecycle of an inhaler is broken down, the user phase and end of life were found to be linked with the highest levels of GHGEs (Janson et al, 2020; Panigone et al, 2020; Jeswani and Azapagic, 2019). Figure 3 offers a visual comparison of these phases, based on a typical pMDl (Jeswani and Azapagic, 2020).

Effective inhaler recycling schemes have the potential to reduce end-of-life GHGEs by 81–87% but sadly there are none currently available in the UK (Panigone et al, 2020; Pernigotti et al, 2021). It was noted from the literature that whilst DPIs contain no propellant, they are responsible for ecotoxicity of plant and aquatic life if disposed of in general waste (Jeswani and Azapagic, 2020). When the new propellant HFA-152a becomes available, significant reductions to end of life phase will occur as not only will emissions be significantly lower, but it will also eliminate the increased risks of ecotoxicity associated with DPIs (Pernigotti et al, 2021).
The safest way to dispose of inhalers is to return them to the pharmacy for incineration. However, at present only 1% of inhalers are disposed of in this way within the UK (Wilkinson et al, 2019; Pernigotti et al, 2021; Murphy et al, 2023). Evidence shows a large reason for this is patients and health professionals being unaware of how to dispose of inhalers correctly (Panigone et al, 2020; Twigg et al, 2019). In addition, it was found that 48% of pMDI and 27% of DPI devices are disposed of with doses remaining (Wilkinson et al, 2019; Murphy et al, 2023; Twigg et al, 2019).
Discussion
Reducing the effect of pMDI
Current pMDIs have a much higher GWP than DPI. However, not all patients with asthma are suited to DPI devices; namely children, the elderly or some adults who may struggle with the inspiratory technique required (Keeley and Partridge, 2019).
It is therefore vital that pMDIs are still made available. The GWP of these inhaler types can still be reduced by avoiding the use of Ventolin evohaler, Flutiform and Symbicort evohaler (devices containing the highest GWP propellent HFA-227ea) and using alternatives such as Salamol pMDI with HFA-134a diluted and Fostair pMDI which uses HFA-134a (Wilkinson et al, 2019, Twigg et al, 2019; British Thoracic Society, 2019). Also, prescribing the higher strength version of preventer inhalers so that one puff rather than two is required will half GHGEs as well as simplify instructions and reduce the number of prescriptions required, the number of trips to the pharmacy and the number of inhalers requiring incineration (Twigg et al, 2019).
New HFA-152a propellant: Do we wait?
The development of this new propellant will ensure that pMDIs remain an option for those that need or prefer it and there are some that argue whether we should wait to make inhaler changes once it has been released (Pernigotti et al, 2021). Certainly, this report has shown that switching to the lower GWP propellant will create the largest GHGEs savings, with the CF of pMDIs predicted to reduce by as much as 90% (Jeswani and Azapagic, 2019). In addition, there are concerns over switching inhaler devices purely for environmental reasons when disease is stable as HCPs have a duty of care to put the patient first (European Respiratory Society, 2021). However, transitioning to novel propellants takes time to fully complete and therefore it is likely there are some years to pass yet before implementation of the new low GWP propellant has taken full effect (Woodcock et al, 2022).
Benefits of DPI
For those that can make a switch to DPI, there is overwhelming evidence to suggest that this not only significantly reduces GHGEs but is also linked with improved asthma control and is generally favoured by both HCPs and patients. In addition to the Salford Lung Study and the non-interventional switch study conducted by Vinge et al in 2020, there have been other reports that have concluded the same. Sanchis et al. conducted a large systematic review in 2016 that found fewer errors were associated with DPI. Price et al (2019) and Galffy et al (2019) both studied clinical effectiveness of switching pMDI to DPI and again observed compelling improvement to disease control and user satisfaction in the DPI groups. Even in emergency situations, DPIs have been found to be as effective in managing symptoms as MDI+spacer or nebulisers (Kponee-Shovein et al, 2022). As a result, the Primary Care Respiratory Society (PCRS) have formally supported suggestions regarding the issuing of ‘rescue packs’ containing a salbutamol pMDI+spacer, so that a move to DPI use in mild-to-moderate exacerbations can be made. This move addresses the concern that patients may not have the inspiration capability required by DPI in severe exacerbation scenarios (Keeley and Partridge, 2019).
The safest way to dispose of inhalers is to return them to the pharmacy for incineration. However, at present only 1% of inhalers are disposed of in this way within the UK «
How to change
Encouraging blanket inhaler switches is not best practice nor based on evidence, and opposes the gold standards for change (Attar-Zadeh et al, 2021). Non-consensual inhaler switches have been linked to a greater number of negative outcomes for the patient, healthcare services and the environment (Chrystyn, 2005; Price et al, 2011). The adverse effects created by such changes include treatment failure, reduced adherence, and increased need for reliever medication (Thomas et al, 2009; Doyle et al, 2010).
Three key elements are involved in successful, gold standard inhaler changes: inhaler technique, patient preference and patient adherence. Correct technique is vital to ensure adequate disposition of medication in the airways, and evidence shows this is more effective when a visual demonstration is offered, rather than written instruction (Schulte et al, 2008). Patient preference is linked to improved adherence and disease control (Wilson et al, 2010). Research has shown that patients’ preferences for one inhaler over another are ease of use and efficacy (Molimard and Colthorpe, 2015; Starup-Hanson et al, 2020) – both qualities commonly related to DPI devices.
Finally, adherence to preventer inhaler regimes results in reduced need for emergency services and less salbutamol prescriptions (Williams et al, 2004). One of the most common reasons for non-adherence is the prescribing of an inhaler that is not the patient's choice, a link commonly associated with non-consensual switches (Horne et al, 2007).
Recycling
It is vital that inhalers are disposed of correctly to prevent propellants leaking into the atmosphere causing ecotoxicity of plant and aquatic life (BJGP Life, 2021). However, with just 1% of inhalers being returned to pharmacies, at present safe disposal requires better training and education for both health professionals and patients (Panigone et al, 2020; BJGP Life, 2021). Studies show that pharmacies and patients would be willing to take part in the safe disposal of and recycling of inhalers if such schemes were to be available (Liatsikos et al, 2021). It appears that if the NHS is to meet its sustainability targets, promotion of safe inhaler disposal through patient education and financial investment to set up inhaler recycling schemes are needed (Liatsikos et al, 2021).
Conclusion
Climate change is a pressing issue of our time, and a move to more sustainable solutions to treat adults with asthma is required. There are several ways in which this can be achieved, including switching pMDI to DPI where possible, avoiding inhalers containing HFA-152ea, altering dose levels to reduce the number of puffs required, using salbutamol DPI for mild-moderate exacerbations, and improving disease control.
Sustainable inhaler changes offer a balance between disease control, patient health and environmental effects, and general practice offers the ideal platform to promote and apply these changes. By working together with asthma patients and involving them in inhaler decision-making, it is possible to lower the carbon footprint of inhalers and optimise disease control. Applying these changes to practice are vital if we are to meet government targets, and protect the future of our planet for generations to come.

