Scarlet fever, also known as scarlatina, is an infectious illness caused by Streptococcus pyogenes (group A streptococcus) (Alotaibi et al, 2022). This is a notifiable disease and there were 12 176 cases of scarlet fever in England between 1 January and 24 March 2024 (UK Health Security Agency, 2024).
Scarlet fever is spread by aerosol transmission or direct contact. All age groups can be affected by scarlet fever but, generally, this illness occurs between the ages of 2 and 8 years (UK Health Security Agency, 2019).
Symptoms
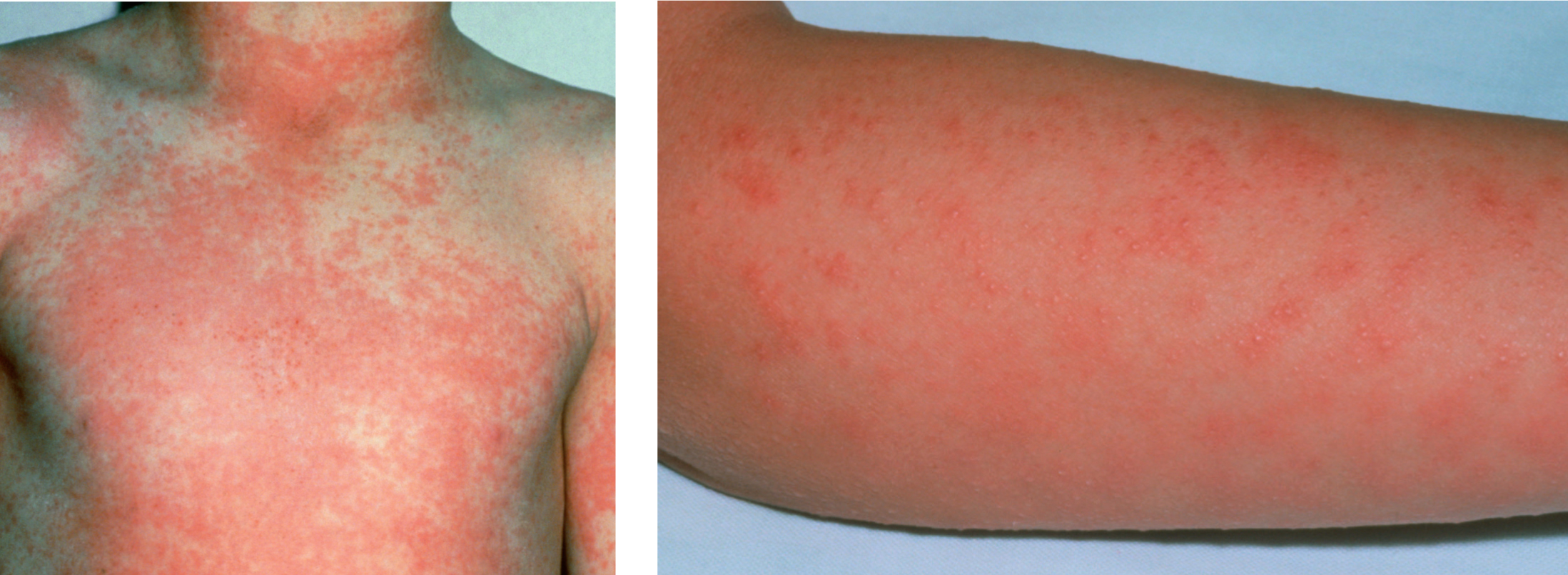
The symptoms of scarlet fever include (NHS, 2025):
Risks and complications
Timely treatment is required to reduce the risk of potential complications and spread of infection (NICE, 2024). If left untreated, scarlet fever can cause more serious complications known as invasive group A streptococcal (iGAS) infection.
This includes necrotising fasciitis, which destroys muscles, fat and skin, and streptococcal toxic shock syndrome, which can cause organ failure (UK Health Security Agency, 2023). Those at greater risk of iGAS include (NICE, 2024):
Diagnosis and management
Scarlet fever is ordinarily diagnosed through GP review of symptoms alone. Throat swabs and blood tests can also be used to make a definitive diagnosis. However, even with mild cases of scarlet fever, a 10-day course of antibiotics is prescribed. Current guidance advises that children should not return to school or nursery, and adults should not work until a minimum of 24 hours after starting antibiotic treatment to reduce the risk of spreading infection (UK Health Security Agency, 2024). If antibiotics are not administered, the infection can spread for 2–3 weeks after symptoms commence.
To avoid spreading scarlet fever, good hand hygiene is advised, in addition to covering the mouth and nose when coughing or sneezing. It is also advisable to not share cutlery, cups, towels, clothes, bedding or baths with anyone who has scarlet fever (NHS, 2025). Self-help strategies include keeping hydrated with fluids, and consuming soft foods if experiencing a sore throat, in addition to antihistamine and antipyretics as required.